What is Crohn’s disease?
What is Crohn’s disease?
Crohn’s disease and ulcerative colitis are the illnesses called inflammatory bowel disease (IBD) . These two diseases are very much alike.
In Crohn’s disease, inflammation can be found in the lining of the intestine. It can also involve the whole thickness of the bowel wall. Crohn’s disease is usually in the lower part of the small intestine, called the ileum. However, it can affect any part of the digestive tract, from where food is taken in (the mouth) to where food comes out (the anus).
Ulcerative colitis only affects the colon. The inflammation can cause pain. It can also make the colon empty often, which causes diarrhea.
Some patients with Crohn’s disease have long periods of remission (when symptoms disappear). This may last months or years. However, there is no way to tell when a remission will happen or when disease symptoms will return. There is no cure for Crohn’s disease so far from Western medicine.
People of all age groups can have Crohn’s disease, but it usually begins in the late teens and early adulthood. Twenty percent of all Crohn’s cases affect children.
Video: What is Crohn’s Disease?
The disease affects males and females equally, but Crohn’s disease tends to run in families and certain ethnic groups. About twenty percent of people with Crohn’s disease have a blood relative with some type of IBD. For those patients with a family history, it is very likely that Crohn’s disease will begin in the teens and twenties.
Causes of Crohn’s Disease
The cause of Crohn’s disease is unknown. Some scientists suspect that infection by certain bacteria, such as strains of mycobacterium, may be the cause of Crohn’s disease. To date, however, there has been no convincing evidence that the disease is caused by infection. Crohn’s disease is not contagious. Although diet may affect the symptoms in patients with Crohn’s disease, it is unlikely that diet is responsible for the disease.
Activation of the immune system in the intestines appears to be important in IBD. The immune system is composed of immune cells and the proteins that these immune cells produce. Normally, these cells and proteins defend the body against harmful bacteria, viruses, fungi, and other foreign invaders. Activation of the immune system causes inflammation within the tissues where the activation occurs. Inflammation is an important mechanism of defense used by the immune system.
Normally, the immune system is activated only when the body is exposed to harmful invaders. In patients with IBD, however, the immune system is abnormally and chronically activated in the absence of any known invader. The continued abnormal activation of the immune system results in chronic inflammation and ulceration. The susceptibility to abnormal activation of the immune system is genetically inherited. Thus, first degree relatives (brothers, sisters, children, and parents) of patients with IBD are more likely to develop these diseases. Recently a gene called NOD2 has been identified as being associated with Crohn’s disease. This gene is important in determining how the body responds to some bacterial products. Individuals with mutations in this gene are more susceptible to developing Crohn’s disease.
Symptoms
Persistent diarrhea (loose, watery, or frequent bowel movements), crampy the digestive tractabdominal pain, fever, and, at times, rectal bleeding: These are the 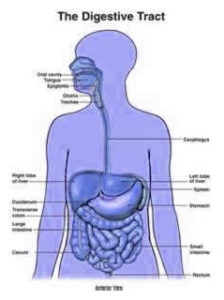 hallmark symptoms of Crohn’s disease, but they vary from person to person and may change over time. Loss of appetite and subsequent weight loss also may occur. However, the disease is not always limited to the GI tract; it can also affect the joints, eyes, skin, and liver. Fatigue is another common complaint. Children who have Crohn’s disease may suffer delayed growth and sexual development.
hallmark symptoms of Crohn’s disease, but they vary from person to person and may change over time. Loss of appetite and subsequent weight loss also may occur. However, the disease is not always limited to the GI tract; it can also affect the joints, eyes, skin, and liver. Fatigue is another common complaint. Children who have Crohn’s disease may suffer delayed growth and sexual development.
Some patients may develop tears (fissures) in the lining of the anus, which may cause pain and bleeding, especially during bowel movements. Inflammation may also cause a fistula to develop. A fistula is a tunnel that leads from one loop of intestine to another, or that connects the intestine to the bladder, vagina, or skin. Fistulas occur most commonly around the anal area. If this complication arises, you may notice drainage of mucus, pus, or stool from this opening.
Symptoms may range from mild to severe. Because Crohn’s is a chronic disease, patients will go through periods in which the disease flares up, is active, and causes symptoms. These episodes are followed by times of remission — periods in which symptoms disappear or decrease and good health returns. In general, though, people with Crohn’s disease lead full, active, and productive lives.
Diagnosis of Crohn’s Disease
A thorough physical exam and a series of tests may be required to diagnose Crohn’s disease.
Blood tests may be done to check for anemia, which could indicate bleeding in the intestines. Blood tests may also uncover a high white blood cell count, which is a sign of inflammation somewhere in the body. By testing a stool sample, the doctor can tell if there is bleeding or infection in the intestines.
The doctor may do an upper gastrointestinal (GI) series to look at the small intestine. For this test, the patient drinks barium, a chalky solution that coats the lining of the small intestine, before x-rays are taken. The barium shows up white on x-ray film, revealing inflammation or other abnormalities in the intestine.
The doctor may also do a colonoscopy. For this test, the doctor inserts an endoscope — a long, flexible, lighted tube linked to a computer and TV monitor — into the anus to see the inside of the large intestine. The doctor will be able to see any inflammation or bleeding. During the exam, the doctor may do a biopsy, which involves taking a sample of tissue from the lining of the intestine to view with a microscope.
If these tests show Crohn’s disease, more x-rays of both the upper and lower digestive tract may be necessary to see how much is affected by the disease.
Complications of Crohn’s Disease
The most common complication of Crohn’s disease is obstruction or blockage of the intestine due to swelling and the formation of scar tissue. The result is thickening of the bowel wall and a significantly narrowed intestinal passage. Symptoms of intestinal obstruction include crampy pain around the mid-abdomen, frequently associated with vomiting. The abdomen may also become bloated and distended. Medications may relieve the obstruction by reducing the local area of inflammation, but surgery may be required if the obstruction is severe and does not respond to medical treatment. Surgery may also be indicated if the blockage recurs frequently.
Another complication is sores or ulcers within the intestinal tract. Sometimes these deep ulcers turn into tracts — called fistulas — that connect different parts of the intestine. But fistulas may also tunnel into surrounding tissues such as the bladder, vagina, or skin. These abnormal passages, which affect about 30 percent of people with Crohn’s disease, often become infected. If the fistula is small, medical treatment may be sufficient to heal it. Large or multiple fistulas, on the other hand, may signal the need for surgery, particularly if they are accompanied by fairly persistent symptoms, such as fever or abdominal pain. Occasionally a fistula forms an abscess, or collection of pus, near the intestine. This is a pocket of infection that requires drainage either through a catheter inserted by a radiologist or a special drain that is surgically inserted. The areas around the anus and rectum are often involved. In addition to fistulas, cracks or fissures may also develop in the lining of the mucus membrane of the anus.
Another type of complication commonly encountered in people with Crohn’s disease is related to malnutrition or the presence of nutritional deficiencies. These are deficiencies of proteins, calories, and vitamins. They generally do not develop unless the disease is extensive and of long duration, conditions that may contribute to inadequate dietary intake and poor absorption of nutrients. Medical treatment is usually effective in the replacement of nutrients. For example, a deficiency in vitamin B-12 can be corrected by an injection of this vitamin. Similarly, an iron deficiency can be reversed by taking this mineral in liquid or tablet form. Nutritional supplements, containing both vitamins and minerals, are available in concentrated form.
Treatment for Crohn’s disease depends on the location and severity of disease, complications, and response to previous treatment. The goals of treatment are to control inflammation, correct nutritional deficiencies, and relieve symptoms like abdominal pain, diarrhea, and rectal bleeding. Treatment may include drugs, nutrition supplements, surgery, or a combination of these options. At this time, treatment can help control the disease, but there is no cure from Western medicine.
Some people have long periods of remission, sometimes years, when they are free of symptoms. However, the disease usually recurs at various times over a person’s lifetime. This changing pattern of the disease means one cannot always tell when a treatment has helped. Predicting when a remission may occur or when symptoms will return is not possible.
Someone with Crohn’s disease may need medical care for a long time, with regular doctor visits to monitor the condition.
Drug Therapy
- Aminosalicylates and corticosteroids are the backbone of treatment for acute attacks.
- Severe attacks require admission to hospital and treatment with intravenous corticosteroids.
- Immunosuppressants, such as azathioprine (eg Imuran) or ciclosporin (Neoral) , are sometimes used for very severe symptoms that have not responded sufficiently to intravenous corticosteroids. (This is an unlicensed indication for these medicines.)
- Aminosalicylate or corticosteroid enemas or suppositories are introduced into the rectum to reduce inflammation in acute mild to moderate disease affecting the rectum or lower part of the intestine.
- Disease that is more widespread in the intestine, or is unresponsive to rectal treatment, requires oral treatment to reduce the inflammation in the intestinal wall. Mild disease is treated with aminosalicylate tablets. More moderate disease requires corticosteroid tablets.
- Infliximab (Remicade) is used for very severe disease that is not improved by treatment with corticosteroids or immunosuppressants.
- Antibiotics are used if there is an additional bacterial infection.
- Vitamin supplements are used in cases where blood samples have shown a lack of one or more vitamins.
- Medicines to treat diarrhoea can be used if this is a major problem.
- Nutritional support may be required during active phases, for example with ‘elemental’ diets that consist of very easily digested food products.
Nutrition Supplementation
The doctor may recommend nutritional supplements, especially for children whose growth has been slowed. Special high-calorie liquid formulas are sometimes used for this purpose. A small number of patients may need periods of feeding by vein. This can help patients who need extra nutrition temporarily, those whose intestines need to rest, or those whose intestines cannot absorb enough nutrition from food.
Surgery
Surgery to remove part of the intestine can help Crohn’s disease but cannot cure it. The inflammation tends to return next to the area of intestine that has been removed. Many Crohn’s disease patients require surgery, either to relieve symptoms that do not respond to medical therapy or to correct complications such as blockage, perforation, abscess, or bleeding in the intestine.
Some people who have Crohn’s disease in the large intestine need to have their entire colon removed in an operation called colectomy. A small opening is made in the front of the abdominal wall, and the tip of the ileum is brought to the skin’s surface. This opening, called a stoma, is where waste exits the body. The stoma is about the size of a quarter and is usually located in the right lower part of the abdomen near the beltline. A pouch is worn over the opening to collect waste, and the patient empties the pouch as needed. The majority of colectomy patients go on to live normal, active lives.
Sometimes only the diseased section of intestine is removed and no stoma is needed. In this operation, the intestine is cut above and below the diseased area and reconnected.
Because Crohn’s disease often recurs after surgery, people considering it should carefully weigh its benefits and risks compared with other treatments. Surgery may not be appropriate for everyone. People faced with this decision should get as much information as possible from doctors, nurses who work with colon surgery patients (enterostomal therapists), and other patients. Patient advocacy organizations can suggest support groups and other information resources.
People with Crohn’s disease may feel well and be free of symptoms for substantial spans of time when their disease is not active. Despite the need to take medication for long periods of time and occasional hospitalizations, most people with Crohn’s disease are able to hold jobs, raise families, and function successfully at home and in society.